What is the challenge?
Many primary care practices struggle to provide high-quality care while remaining financially stable. There simply isn’t enough time in the day for busy providers to meet all their patients’ needs. When all aspects of a patient’s care depend upon a single provider it can have a negative impact on both care quality and practice productivity—and can contribute to an inefficient and stressful work environment. Furthermore, provider-dependent practices have difficulty providing the full range of services that improve patient outcomes, such as care coordination or more intensive follow-up of high risk patients. In order to move to a more team-based, efficient, and satisfying model of care, primary care practices will need leadership and a commitment to change the culture from the traditional provider-centered, hierarchical model of practice to a more team-based culture of mutual respect and appreciation for all members of the team.
What needs to change?
Strong evidence indicates that primary care practices should move to a team-based model of care, where care teams explicitly share responsibility for a defined group of patients and have systems to support team-based care. The team can take several forms, but generally includes a core team built around one or a small number of specific providers. The core team collaborates to manage the encounters (visits, e-mail, etc.) generated by patients of their provider(s). In addition to the provider(s), a care team might include one or more medical assistants (MAs), a registered nurse (RN), and one or more administrative staff or other lay-person roles such as health coach or patient advocate. In larger practices, the core teams are supported by an extended team consisting of centralized health professionals and administrative staff. Commonly, professionals include RNs in care management or supervisory roles, pharmacists, and behavioral health specialists. Practices often need to reorganize the work to maximize each team member’s skills and expertise, offload provider tasks, expand the services that can be offered, and use standing orders and predefined workflows that take full advantage of the team structure.
For many reasons, it is useful to engage patients as members of their care team:
- To help patients see the core team as an enhancement to their provider’s care and support, and not a dilution of provider involvement in their care
- To help patients understand the different, complementary skills and roles team members play
- To give patients more opportunities to get questions answered and needs met by individuals with whom they have a relationship
- To help the practice improve the quality and relevance of its care and service
High functioning team-based care requires a change in the provider-focused mental model including explicit efforts to build trust, respect, and value for new roles in the primary care workforce, and for thinking of patients as partners in care.
What do we gain by making these changes?
Involving additional team members in the delivery of chronic illness and preventive care has been repeatedly shown to improve performance measures. Evidence also suggests that team-based care can help primary care practices increase productivity, enhance efficiency, and create a more satisfying work environment. When clinicians and staff work together, a practice is better able to meet patients’ needs and can often increase its capacity to see more patients.
- Identify the leadership for teams and start building a team culture
Even before you begin building your team, it’s important to identify clear leadership for this change and start developing a culture that supports teamwork. It is a culture that empowers and prepares staff to take on new roles and act independently, encourages providers to give up tasks done better or more efficiently by others, and encourages communication. Strategies that LEAP sites have found helpful include:
- Ensure that formal and informal practice leaders repeatedly voice clear and strong support for team-based care, and act consistently in a way that signals their support for this model.
- Dedicate resources for team-building exercises to help team members begin developing trust and a coordinated way of working together.
- Locate core team members in close proximity with each other. Several LEAP sites had team rooms or team spaces where providers and core team staff did their charting and telephoning.
- Encourage daily huddles and meetings to organize the work and solve problems together.
Flatten the hierarchy by encouraging all member of the team to have a voice in discussions, explicitly sharing performance information and credit (e.g., performance bonuses) for successes with all members of the team.
- Develop a core team structure or structures that you think will meet the needs of your patients and providers, AND TEST IT
No single core team structure appeared superior to others. Some LEAP sites built their core teams around a single provider (e.g. a teamlet with 1 provider and 1 or 2 MAs) and some built multi-provider teams (e.g., 2-3 providers, 2-3 MAs, 1 RN). Smaller core teams may make it easier for staff to develop relationships with patients. The extended team in most LEAP sites included RN care managers, behavioral health specialists, and pharmacists. These additional professionals could be employees of the clinic or supported by an affiliated organization such as a health plan, community mental health center, or academic institution. Administrative staff could be centralized and/or linked with a core team.
- Develop clear roles and responsibilities for every member of the team
These should ensure that each team member is working to the top of their skillset and credentials. This most often means expanding the roles of additional staff members to take on tasks previously done by providers or not done at all. For example, preventive care procedures (e.g., immunizations, ordering cancer screening, assessments such as monofilament foot exams) in most LEAP sites were routinely and independently performed by MAs and/or LPNs. Be sure to research state policies regarding licensure and scope of practice rules for various roles. You may also want to explore state liability regulations.
- Encourage and enable staff to work independently.
- Develop standard work processes for the delivery of common services, and incorporate them into practice workflows and into the Electronic Health Record. Systematizing expanded roles in standard work helps reduce variation and prevent backsliding.
- Maximize the use of standing orders. Standing orders enable staff to independently perform key clinical tasks without having to involve the provider.
- Engage patients as a member of the care team and help them understand what they can expect in a team-based model of care.
Many patients may not be familiar with the team-based approach and do not know what to expect when receiving care from multiple team members or the benefits of having a team around them. It helps to develop simple scripting that clinicians and staff can use to explain that all team members are working together, communicating regularly, and operating under the direction of the patient’s primary care provider.
- Provide team members with regular, dedicated time to meet about patient care, quality improvement, and to facilitate strong working relationships.
While it can be financially and logistically challenging to take staff members “off line,” dedicated time is an essential investment to create high functioning teams that deliver high quality, coordinated care to patients. LEAP sites use a variety of approaches to meetings, including huddles, improvement events, and care conferences.
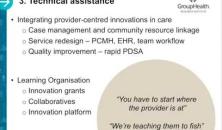
- Provide training so that staff members learn new tasks and how to coordinate with team members.
LEAP sites support team members with strong internal training programs, having found that current educational programs often do not prepare the workforce for a high functioning team model. Many LEAP sites emphasize cross-training so workflows are not interrupted when short-staffed.
- Develop career ladders for staff members in all roles.
Many LEAP sites have been able to hire enthusiastic, talented individuals into relatively low paying roles such as Medical Assistant, Administrative staff, or lay roles such as community health worker, health coach or patient navigator. In an effort to reward excellent performance and keep staff, some sites have found explicit career ladders to be useful.
Publications
Webinar and power point presentations
Video
ToolkitsImplementation guides and other documents with extensive resources included
Role featuresJob descriptions, career ladders and other HR materials
Case summariesVignettes, profiles and testimonial videos
LEAP Learning ModuleOther helpful topics included in this website
Clinical protocolStanding orders, risk stratification forms and hospital transition protocols
Staff trainingTutorials, training manuals, etc.
WorkflowTemplates, flow sheets and mapping aids
Patient materialsAction plans, brochures, team cards, welcome letters
If you have a question about the improvements, action steps, or tools & resources in this module please let us know. We're here to help. And if we can't answer your question, we can probably connect you with someone who can.